[ad_1]

The number of overdoses that involve both fentanyl and stimulants like cocaine and meth is growing fast. One way people who use drugs can protect themselves is by using test strips to check for the presence of fentanyl in other drugs.
Mark Lennihan/AP
hide caption
toggle caption
Mark Lennihan/AP
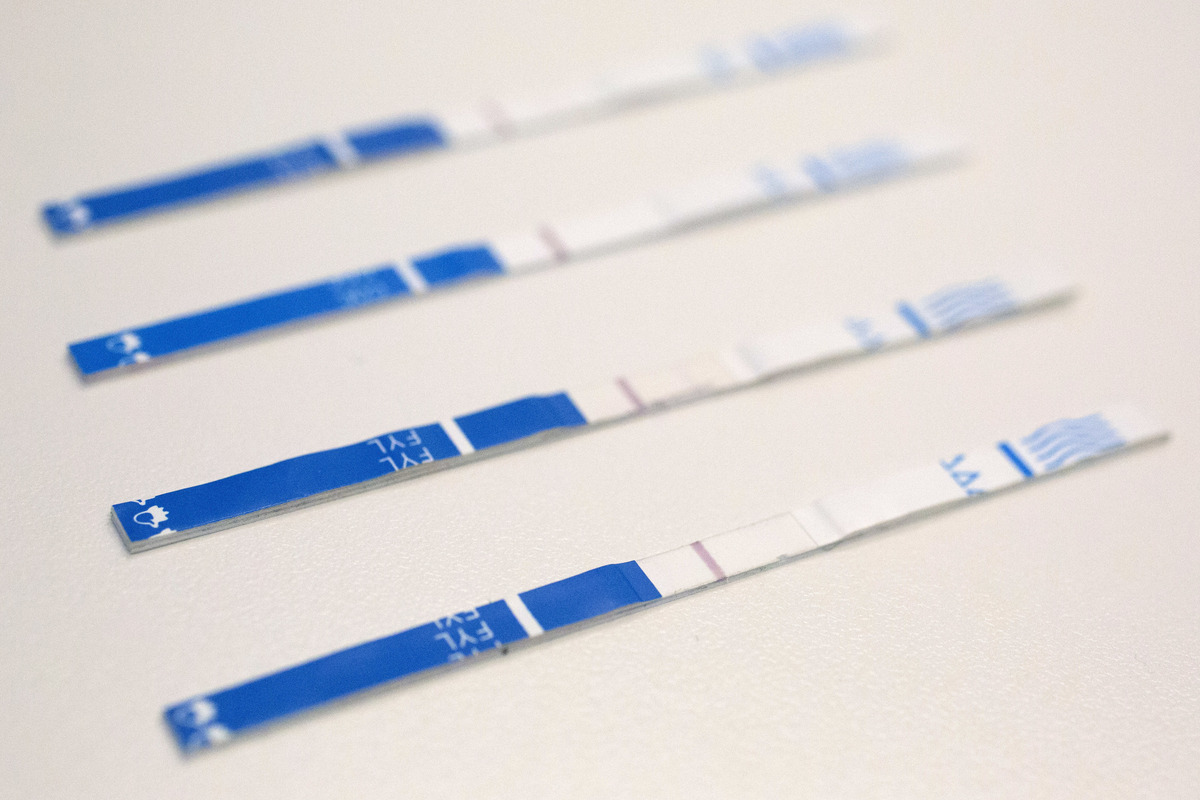
The number of overdoses that involve both fentanyl and stimulants like cocaine and meth is growing fast. One way people who use drugs can protect themselves is by using test strips to check for the presence of fentanyl in other drugs.
Mark Lennihan/AP
The mixture of stimulants like cocaine and meth with highly potent synthetic opioids is a fast-growing driver of fatal overdoses in the U.S.
Since 2010, overdoses involving both stimulants and fentanyl have increased 50-fold, and now account for 32% of U.S. overdoses in 2021 and nearly 35,000 deaths, according to a study published Thursday in the scientific journal Addiction.
“We’re now seeing that the use of fentanyl together with stimulants is rapidly becoming the dominant force in the U.S. overdose crisis,” says Joseph Friedman, the lead author of the study and a researcher at UCLA’s David Geffen School of Medicine. “Fentanyl has ushered in a polysubstance overdose crisis, meaning that people are mixing fentanyl with other drugs, like stimulants, but also countless other synthetic substances.”
The study authors call the rise in these polysubstance overdoses a “fourth” wave in the opioid crisis. The first was characterized by the rise in prescription opioids starting in the early 2000s, the second by heroin’s rise starting around 2010 and the third, fentanyl circa 2013.

Chelsea Shover, the senior author of the paper and assistant professor-in-residence at UCLA, says understanding how people use drugs is crucial to stopping the overdose crisis and helping people get treatment.
Awareness of effective medical treatments for opioid addiction, including drugs like suboxone and methadone, has increased over the years. .
Shover says preventing poly-drug overdoses, “also means getting serious about treating stimulant use disorder.”
“It’s not just an opioid crisis, although all the strategies we’re trying to deal with opioid overdose still apply,” she adds.
However, treatments for stimulant use disorder are still rare and underfunded.
How people are dying
Opioids and stimulants have a history together. People who chronically use opioids often will turn to stimulants as a way to offset the tiredness that comes along with the use of drugs like heroin and fentanyl.
The tactic is called speedballing, according to the National Institute on Drug Abuse, and can cause an intense high, which can also be very dangerous.
“Stimulants cause vasoconstriction of your vessels and increase your need for oxygen,” said Eric Weintraub, the director of addiction research and treatment at the University of Maryland School of Medicine. “Opioids do the opposite, they actually decrease your respiration so less oxygen is delivered to the body.”
That stress on the body can make people more susceptible to an overdose.
Another group of people who are affected are people intending to use stimulants on their own but who don’t realize their supply has been laced with or contaminated with potent drugs like fentanyl.
“The drug supply is so toxic and dangerous, so if somebody’s using cocaine on the weekends here and there and they get the wrong batch, they could die of an overdose as well,” Weintraub said.
Making sense of autopsy data
While taking both of the drugs at the same time is potentially lethal, it’s important to note that just because a person has both stimulants and opioids in their bloodstream, it doesn’t mean they died from the combination.
Autopsy toxicology reports, which the Addiction study is based on, are not a perfect science.
“What they do is just provide us a list of substances that a person may have used, it doesn’t tell us when they used it and doesn’t tell us if they were consumed at the same time,” said Zachary Kosinski, the director of harm reduction at the Behavioral Health System Baltimore. “The sources usually do a pretty poor job of telling us what caused the overdose.”
Shover said that death certificate data has its limitations, but medical examiners are taking note of what may have caused the fatality.
“The deaths that are included in this study, when we say a death involves fentanyl and cocaine, that means that at some point a medical examiner or coroner determined that both were important factors in causing death,” Shover said. “What we can’t know is, did someone use fentanyl and cocaine together on purpose? Did someone use cocaine thinking that it was just cocaine and it had fentanyl in it? We can’t tell that from this type of work.”
She noted that the data point to important trends that can help focus treatment and resources. For example, previous waves hit white and Native American populations particularly hard. However, this new wave is skewing toward the Black population.
There are also geographic considerations. In the northeast, fentanyl tends to be combined with cocaine, while in the south and west it is more likely to be mixed with methamphetamine.
“We suspect this pattern reflects the rising availability of, and preference for, low-cost, high-purity methamphetamine throughout the U.S., and the fact that the Northeast has a well-entrenched pattern of illicit cocaine use that has so far resisted the complete takeover by methamphetamine seen elsewhere in the country,” Friedman said.
Weintraub and Shover said it’s unlikely that people will stop illicit drug use anytime soon, so it’s important that the overdose antidote Narcan is made widely available in places where people use drugs.
This story was produced as part of a reporting partnership with WYPR and KFF Health News.
[ad_2]
Source link



Comments are closed.